
PRONING POSITION SKIN
“Within four hours of the patient being admitted to or coming back to the floor, an assessment of the patient’s skin is completed by two nurses,” Ash says. The four eyes, four hours process was established to provide a regular comprehensive check of the patient’s skin to document and monitor changes to prevent injury. “In addition, deep-tissue injuries can be serious for patients and may require surgical repair as well as increase the risk of mortality.” “We were noticing a lot of pressure injuries on patients coming in from different hospitals that were not getting documented, and the hospital does not get reimbursed for care if an injury is developed within the hospital,” notes ICU Clinical Coordinator Ash Caretti, RN, CCRN, who chairs the CUSP team. The CUSP committee’s role is to assess patient safety and then develop programs or processes to address concerns. “As a nurse, you are constantly learning, and the pandemic has definitely inspired me to continue to increase my knowledge.”īefore the pandemic began, the ICU’s comprehensive unit-based safety program (CUSP) team noticed an increase in pressure injuries. We have worked hard in mastering the process and it has been very impactful in treating our patients.

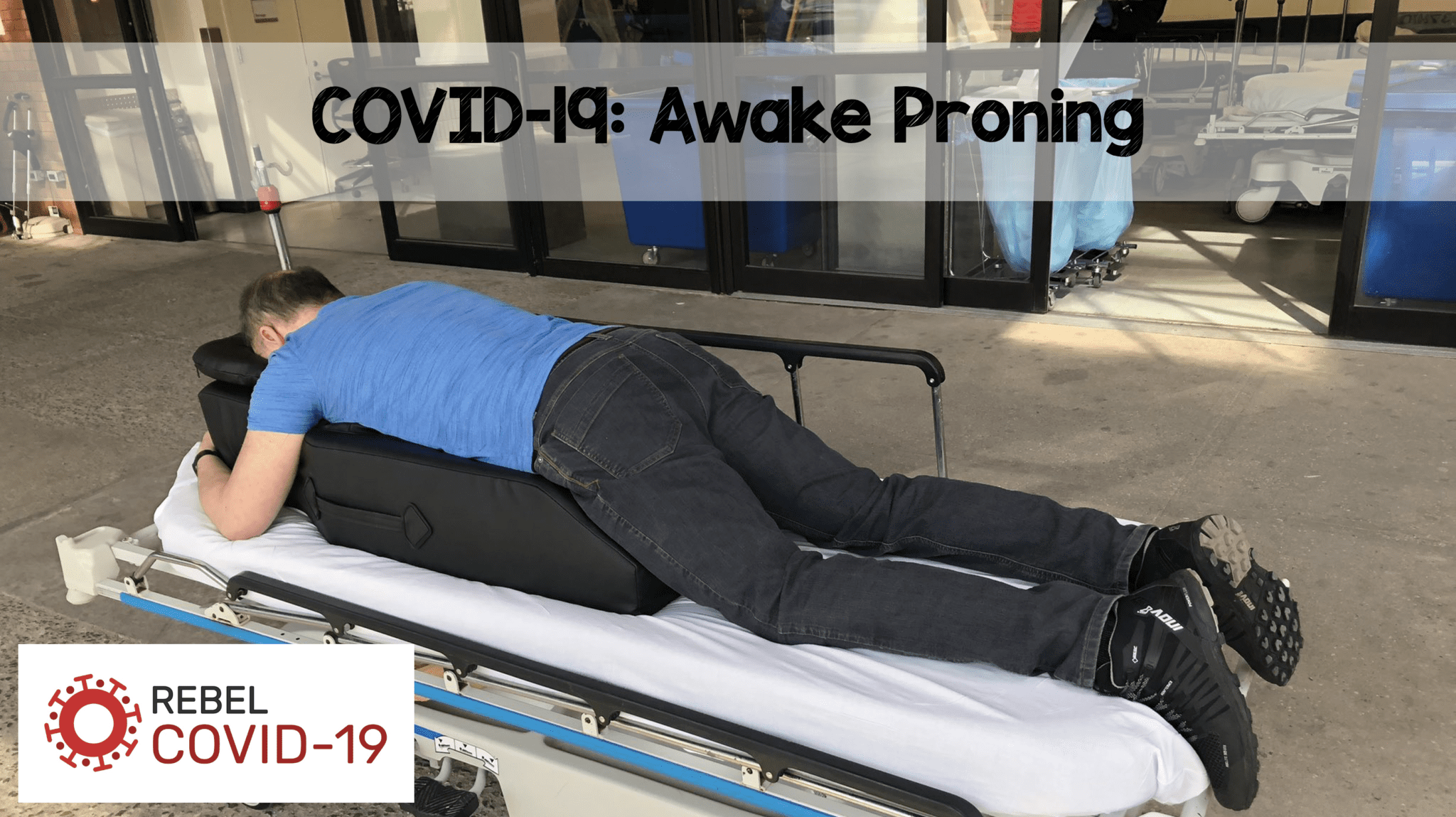
These patients typically stay proned for 16 hours. We then gently and strategically roll them from their back to side and then prone on the stomach. We typically use three team members on either side of the patient and respiratory at the head of the bed to manage the patient’s airway. In our process of proning, the patient is on a flat sheet, we place padding on bony areas and position pillows to protect their chest, pelvis, knees and feet. We have used specialty prone pillows and specialty prone beds to help with the process. “We have tried multiple ways to prone patients. We gathered a multidisciplinary team which included physical therapy, occupational therapy, respiratory therapy and nursing to figure out the best way to do it.
PRONING POSITION MANUAL
HCGH had a manual process, but with the number of patients we were proning, it required a team. When the patient is proned, the position facilitates better ventilation of the posterior lung regions. The purpose of proning is to allow better distribution and volume of air in the lungs. Proning, which is when the patient is placed on their stomach, is a normal standard of care in patients with acute respiratory distress syndrome (ARDS), and the research showed this to be an effective tool with patients with COVID-19.
.png)
“Early research and new studies were being published that provided guidance in the treatment of patients with COVID-19. ICU Clinical Coordinator Ash Caretti, RN, CCRN, explains how the ICU flexed early in the pandemic, as volumes increased and staff learned along the way. Processes and protocols for caring for patients with COVID-19 were changing and evolving constantly. Howard County General Hospital’s ICU was no different. The ICU in most hospitals was ground zero early in the pandemic.


 0 kommentar(er)
0 kommentar(er)
